Pharmacy providers claiming tips
It's easier than you think!
Alberta Blue Cross® is an independent, not-for-profit organization providing health and dental benefits to plan members who work, live or may have retired in your pharmacy’s area. To ensure efficient service to your customers who have drug coverage through Alberta Blue Cross®, we encourage you to take advantage of our direct billing services through our real-time claim adjudication network.
Submitting a claim online to Alberta Blue Cross® is quick, easy and secure. All the information you need is on the customer’s Alberta Blue Cross® ID card. Within seconds, results are displayed confirming the amount the benefit plan pays and any portion your customer is required to pay.
Tips for online claim entry and successful claims adjudication
Download claiming tips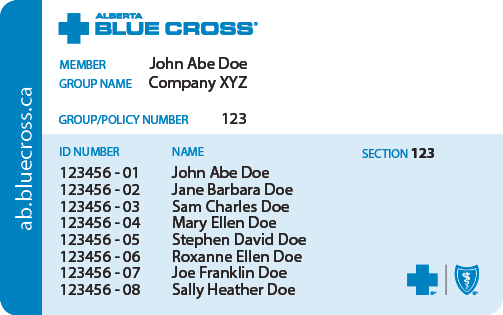
- Carrier Code 11 (Alberta Blue Cross®): is to be used when submitting claims for your customers that have Alberta Blue Cross® employer sponsored direct bill drug coverage.
- Group Number: enter as a seven-digit number (fill with leading zeros if necessary) followed by Section Number (up to three characters, no zero filling). If your software does not utilize a separate field for the section, the group and section are to be entered as one string.
- Identification No: (example 1234567-33) “1234567” enter as a 10 digit number (fill with leading zeros if necessary) followed by “33” the two digit patient code. If your software does not utilize a separate field for the patient code, the Identification No. should be directly followed by a / or – symbol, then the two digit patient code.
- Cardholder (member/subscriber) last name: must be indicated on all claim transmissions along with the patient first and last name.